In the grand tapestry of history, the relationship between humans and animals has been both harmonious and perilous. From eating habits to shared spaces, our interactions with the animal kingdom have sometimes led to outbreaks with potential to change the course of humanity. Here are 13 times animal-driven diseases nearly decimated human populations and what you can learn from these close calls.
1. The Bubonic Plague

The Bubonic Plague, also known as the Black Death, was a pandemic that swept through Europe in the 14th century, killing an estimated 25 million people. The bacterium Yersinia pestis, carried by fleas that lived on rats, was the culprit behind this catastrophic outbreak. As trade routes expanded, so did the reach of this deadly disease, exploiting the close quarters of burgeoning cities. People of the time were unaware of the scientific link between the fleas and the disease, leading to widespread panic and scapegoating.
A study published in The Lancet Infectious Diseases highlights how the plague reshaped societal structures and economies, leading to significant shifts in population dynamics. Understanding the plague’s origins and spread is crucial in modern times, reminding you of the importance of rodent control and public health measures. Essentially, this haunting chapter in history underscores the vulnerabilities in human-animal interactions. It serves as a vivid reminder that even the smallest creatures can wield enormous power over our lives.
2. The H1N1 Swine Flu

In 2009, the H1N1 swine flu pandemic emerged, causing global concern and affecting millions worldwide. Originating in pigs, the virus rapidly spread to humans, thanks to its ability to easily transmit through respiratory droplets. Unlike seasonal flu, H1N1 disproportionately affected young people, causing alarm about its potential impact. You might recall the rush for vaccinations and the heightened hygiene practices that became routine.
The swine flu pandemic highlighted gaps in global health preparedness and the need for swift information dissemination. It taught people to be more vigilant about flu-like symptoms and the importance of vaccination. While less deadly than initially feared, H1N1 served as a stark lesson in how quickly zoonotic diseases can spread. Remembering this event can help guide future responses to similar outbreaks.
3. The Zika Virus

The Zika virus outbreak of 2015-2016 brought the world’s attention to the dangers of mosquito-borne illnesses. Initially discovered in monkeys in the Zika Forest of Uganda, it eventually spread to humans, causing severe birth defects in infants born to infected mothers. The virus primarily spread through the Aedes mosquito, well-known for carrying other tropical diseases. You may recall the widespread travel advisories and concerns, particularly for pregnant women.
According to a report by the World Health Organization, the Zika outbreak highlighted the need for robust vector control strategies and international collaboration. This incident emphasized the interconnectedness of human and animal health and the importance of monitoring emerging infectious diseases. The Zika crisis taught you to be wary of mosquitoes not just for their annoying bites but for their potential to carry life-altering diseases. It’s a reminder to always take precautions, especially when traveling to tropical regions.
4. The Nipah Virus

Emerging in Malaysia in 1998, the Nipah virus was a stark reminder of the dangers posed by zoonotic diseases. It originated from fruit bats but eventually spread to pigs and humans, with devastating effects. The outbreak resulted in severe respiratory and neurologic conditions, prompting swift action to cull infected animals. You might find it chilling that this virus has a high mortality rate and no specific treatment.
The Nipah virus taught crucial lessons in disease surveillance and the importance of early intervention. It also highlighted the need to manage animal farming practices to prevent future spillovers. With its potential for human-to-human transmission, Nipah served as a wake-up call to improve global health systems. This outbreak is a testament to how quickly a disease can escalate and the importance of preparedness.
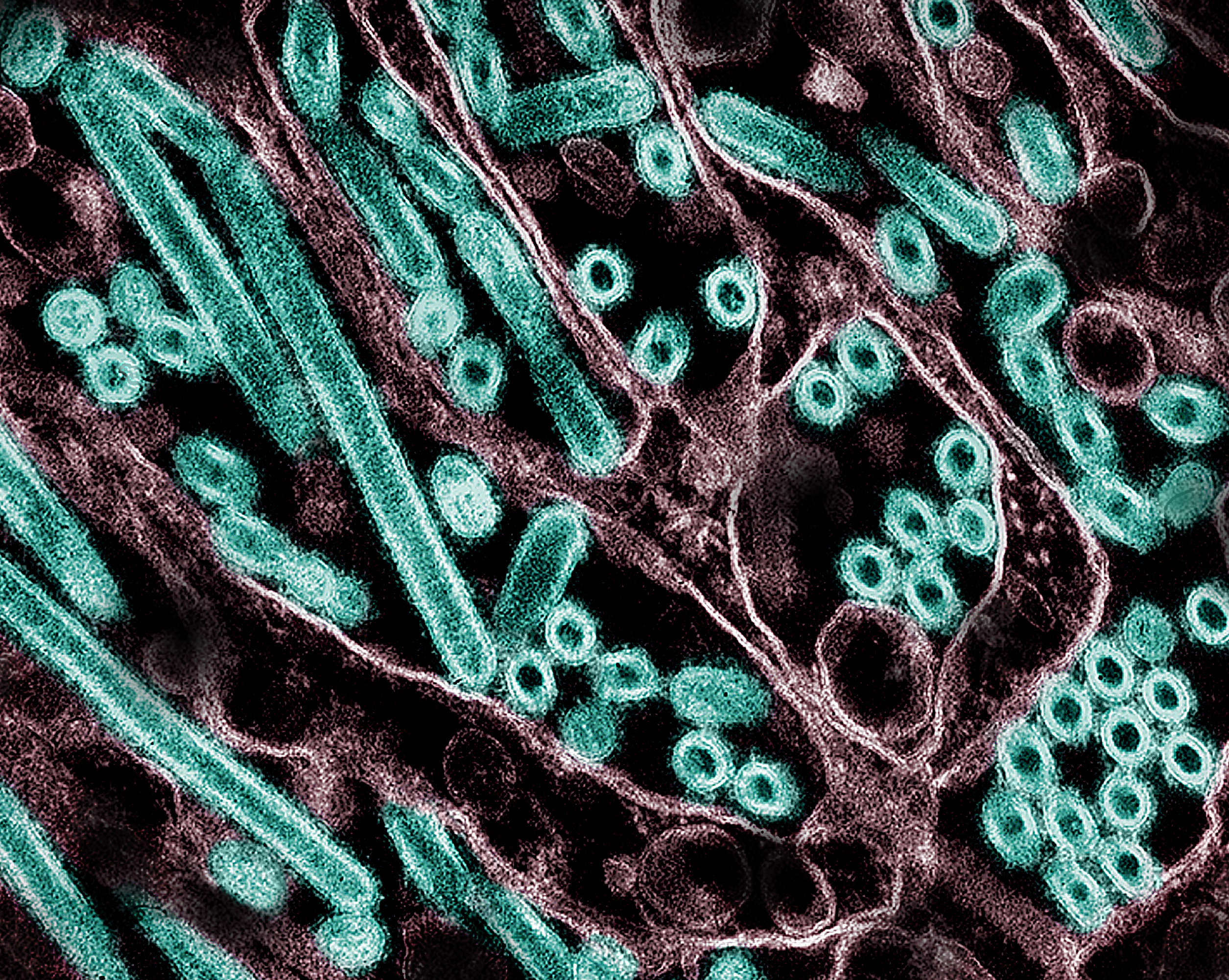
5. The Ebola Virus

Ebola, a name that evokes horror due to its gruesome symptoms and high fatality rate, has its roots in African fruit bats. The 2014-2016 outbreak in West Africa was the largest, infecting thousands and causing widespread fear. The virus spreads through direct contact with bodily fluids, making it particularly dangerous in densely populated areas. You might remember the intense international response and the race to contain the virus before it spread globally.
Research from the Centers for Disease Control and Prevention (CDC) found that early detection and isolation are key to controlling Ebola. This outbreak underscored the critical need for global health systems to be equipped and ready to act swiftly. The Ebola crisis not only highlighted the fragility of health systems in affected regions but also the interconnectedness of global health security. It’s a vivid reminder of why vigilance and cooperation are necessary in the face of emerging diseases.
6. The Avian Influenza (Bird Flu)

Avian influenza, commonly known as bird flu, is a highly pathogenic virus that has periodically made the jump from birds to humans. While the virus primarily affects poultry, certain strains have caused significant human infections, leading to high mortality rates. The H5N1 strain, in particular, has caused concern due to its potential to mutate and spread easily among people. You probably recall hearing warnings about the dangers of close contact with live poultry.
The bird flu outbreaks have prompted significant changes in agricultural practices and monitoring. They have also underscored the importance of controlling animal diseases to prevent human pandemics. Surveillance and rapid response have been key in managing these outbreaks. This situation serves as a reminder of how interconnected our health is with the animal kingdom.
7. The HIV/AIDS Epidemic

The HIV/AIDS pandemic, which has claimed millions of lives since the late 20th century, is believed to have originated from primates in West Africa. The virus made the jump to humans through the hunting and consumption of bushmeat. Once in the human population, HIV spread rapidly due to a combination of biological and social factors. You might recall the initial stigma and misconceptions surrounding the disease, which hampered early responses.
A pivotal study published in Science traced the origins of HIV to a specific region in Cameroon, highlighting how zoonotic diseases can have far-reaching impacts. The HIV/AIDS crisis revolutionized public health, leading to improvements in disease surveillance, treatment, and international collaboration. It serves as a somber reminder of the long-lasting effects that animal-borne diseases can have on human populations. This pandemic has fundamentally changed our approach to global health and disease prevention.
8. The SARS (Severe Acute Respiratory Syndrome) Outbreak
SARS, which emerged in China in 2002, was a wake-up call for the world about the dangers of coronaviruses. Believed to have originated in bats before spreading to civet cats and then humans, SARS spread rapidly across continents. The virus caused severe respiratory illness with a notable fatality rate, leading to widespread fear and economic disruption. You might remember the intense public health measures, including travel restrictions and quarantine protocols.
The SARS outbreak highlighted the importance of transparent communication and international cooperation in managing infectious diseases. It also spurred advancements in virology research and vaccine development. In many ways, SARS set the stage for how the world would later respond to COVID-19. This outbreak taught us the value of preparedness and the need to monitor animal populations closely.
9. The MERS (Middle East Respiratory Syndrome) Pandemic

MERS, another coronavirus, emerged in the Middle East in 2012, primarily transmitted from camels to humans. The virus caused severe respiratory illness with a high mortality rate, sparking concerns about its potential to become a global threat. While human-to-human transmission was limited, the sporadic outbreaks caused significant alarm. You may recall the heightened precautions taken in healthcare settings to prevent its spread.
MERS underscored the importance of understanding the animal reservoirs of infectious diseases. It highlighted the need for increased surveillance and research into zoonotic diseases. The outbreak also served as a reminder of the challenges of containing diseases in regions with limited healthcare infrastructure. It emphasizes the need for vigilance and rapid response to emerging health threats.
10. The Rise of Lyme Disease

Lyme disease is a bacterial infection transmitted to humans through the bite of infected black-legged ticks. First identified in the 1970s, the disease has become the most common vector-borne illness in the United States. You might know someone who’s been affected by its flu-like symptoms and characteristic bullseye rash. While not as immediately deadly as other outbreaks on this list, Lyme disease can have serious long-term effects if untreated.
The increasing prevalence of Lyme disease is linked to changing environmental conditions and expanding tick populations. It highlights the complexity of disease ecology and the interplay between human activity and wildlife. The rise of Lyme disease calls for improved public awareness and preventive measures. It serves as a reminder of how even small creatures can impact human health in significant ways.
11. The Mad Cow Disease (BSE) Panic

Bovine Spongiform Encephalopathy (BSE), commonly known as mad cow disease, emerged in the UK in the 1980s, causing widespread panic. The disease is a fatal neurodegenerative disorder in cattle, which can be transmitted to humans through the consumption of contaminated beef, leading to variant Creutzfeldt-Jakob disease (vCJD). You might still be wary of eating beef from certain regions due to this past scare. Although relatively rare in humans, the disease’s severe and fatal nature caused significant alarm.
Mad cow disease highlighted the critical importance of food safety regulations and monitoring in the meat industry. It led to significant changes in cattle farming practices and the implementation of rigorous testing protocols. The incident underscored the potential risks associated with agriculture and food production. It serves as a cautionary tale about the need for vigilance in safeguarding the food supply.
12. The Rabies Infection

Rabies is a viral disease that has been known to humans for centuries, transmitted through the bite of infected animals, most commonly dogs. Despite the availability of vaccines, rabies remains a significant public health issue in many parts of the world. The disease is almost always fatal once symptoms appear, making prevention through vaccination and immediate post-exposure treatment crucial. You might have been advised to get a rabies shot if traveling to certain regions.
The persistence of rabies highlights the challenges of controlling zoonotic diseases in countries with limited resources. It underscores the importance of animal vaccination programs and public education. Rabies serves as a reminder of the ongoing need for global health initiatives to address preventable diseases. It emphasizes that even age-old threats continue to pose challenges today.
13. The West Nile Virus

West Nile Virus, primarily transmitted through mosquito bites, emerged in the Western Hemisphere in 1999, causing significant concern. The virus, which originated in birds, can lead to severe neurological disease in humans, although most cases are asymptomatic. Public health campaigns have focused on mosquito control and reducing standing water where mosquitoes breed. You might have participated in community efforts to curb mosquito populations during peak months.
The spread of West Nile Virus serves as a reminder of the adaptability and resilience of mosquito-borne diseases. It highlights the need for ongoing surveillance and public health strategies to mitigate the risks posed by mosquitoes. The virus underscores the interconnectedness of ecosystems and the impact of environmental changes on disease dynamics. It serves as a call for continued research and innovation in disease prevention and control.
